I wake up in this hospital room. I don’t feel any pain. Is it the effects of the anesthesia or simply the joy of knowing that the uterine fibroids have finally been removed? I don’t know. My uterus has been slit. More than a dozen fibroids have been removed. More than three hours under general anesthesia. Now my recovery begins. I feel free.
Stage 1: It’s nothing, just benign, non-cancerous tumors. I have no pain and many black women do.
In 2014, during an ultrasound following pelvic pain, the doctor informed me that I had uterine fibroids.
Me: “What are they?”
Him: “These are benign tumors located in the uterus“.
Me: “Is it dangerous?”
Him: “No, many black women are carriers of fibroids”.
Benign tumors. Not cancerous. Many black women have them. I have no pain. OK, it’s nothing!
Having as precept “It is better to prevent than to cure”, every year, I take an ultrasound test. The 3 subserous fibroids increase. But I am assured that it is still nothing! I have no symptoms.
At the end of 2016, I meet Aïssatou, from Fibromelles (now the Vivre 100 fibromes association) who campaigns for knowledge of uterine fibroids. She tells me about her experience. We are several women there listening to her. Two or three say they have uterine fibroids.
Aïssatou’s sentence remains etched in my mind: “We are often asked to feel our breasts for control purposes. Why aren’t we asked to feel our belly to detect the presence or absence of an abnormal abdominal mass?”
Motivated by the fight of this woman who campaigns for women’s health, I decide to join the Vivre 100 Fibromes association. There, I discover more and more this disease. I have no idea that these muscle cells will lead me to undergo the first operation of my life. But they don’t seem so benign anymore. The numbers speak:
- 30% of uterine ablations in Canada are due to uterine fibroids.
- 30 to 50% of women are carriers of fibroids
- Up to 80% of black women and 70% of white women
I feel lucky because unlike some women, I have none of the pain:
- No painful and abundant periods
- No pain during intercourse
- No abdominal swelling.
I am what is known in medical jargon as “asymptomatic” (having no clinical symptoms). Nevertheless, some fibroids continue to grow and one of the fibroids is now almost 9 centimeters in diameter, about the size of a 14-week-old embryo. I’m still lucky not to have the belly of a 14-week pregnant woman.
Following my principle “It is better to prevent than to cure” and knowing that everything that is not expressed leaves its imprint, I seek to understand the cause of my illness.
My illness – Evil ness – is trying to tell me something. In Ayurveda and in many other medical precepts, the uterus is the symbol of femininity, creativity, fertility, a place of memory… It connects us to our feminine power. So, what has not been expressed?
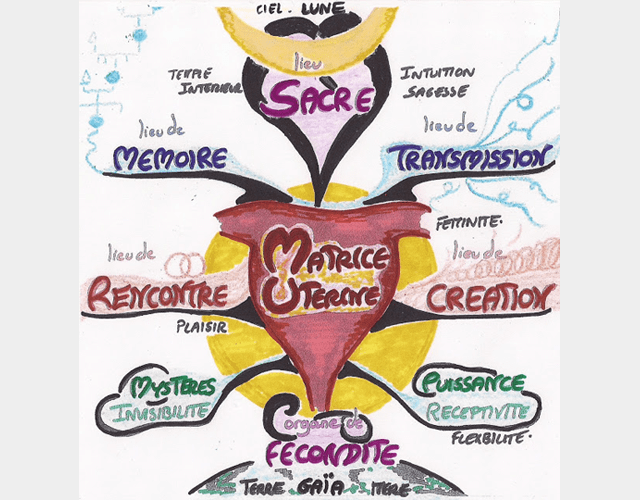
Source: http://www.1001fecondites.com/2011/10/matrice-uterine-berceau-de-fecondite-et.html
In order to better understand my menstrual cycle, I download an application to list all the symptoms during my period; very useful when gynecologists ask me questions about my cycle. I also follow a training with Séréna Québec on the symptothermal method which allows you to identify the fertile and infertile periods of the cycle. Having a better knowledge of my body and becoming aware of all the little changes that occur during my cycle is very beneficial.
I consult a naturopath, an osteopath, and an acupuncturist. I modify my diet and favour organic foods as much as possible, consuming more raw vegetables, avoiding industrial milks and tea. Milk thistle, which helps support liver activity, becomes a friend of mine. Following the recommendations of my acupuncturist specialized in fertility (gynecologist in her country of origin), I start drinking warm or room temperature water. This helps stimulate natural digestive enzymes and improve digestion.
In addition to sports, which I do regularly, I add the practice of yoga.
I won’t say it has a direct effect on the bigger fibroids, but I’m sure it helps my well-being and that of my uterus and prevents some of the fibroids from growing.
Phase 2: Pain, Stress and Medical wandering.
During the summer of 2017, a friend asks me if I was pregnant. No! My belly has swelled. My bladder is under increasing pressure from the fibroids. My sleep is frequently interrupted by this discomfort. I go from asymptomatic to symptomatic.
From September to November 2017, I perform 2 ultrasounds. I make 2 medical visits to 2 different gynecologists. At each appointment, I bring all my ultrasounds (very important when you don’t have a family doctor). My goal: to find an understanding doctor who agrees to follow me and perform a myomectomy. This surgical procedure under general anesthesia consists of removing uterine fibroids. Unlike hysterectomy, the uterus is preserved.
The first gynecologist gives me a prescription for an MRI (Magnetic Resonance Imaging), but in the meantime recommends that I take Fibristal, then do the MRI afterwards. This medication may cause fibroids to shrink by blocking the effects of progesterone on the endometrium. You should know that progesterone is a hormone that stimulates the formation and growth of fibroids. Given the listed side effects and the minimal likelihood of it having an effect on my large fibroids, I decide not to take this medication. Eager to have a second opinion, I consult a gynecologist. She does not consider my case alarming because my symptoms are not significant. Nevertheless, she prescribes me a pelvic ultrasound.
At the beginning of December, I am back with this 2nd gynecologist. After hearing my argument, she finally agrees to put me on the hospital’s waiting list for a myomectomy which will probably take place in the next 6 months.
On January 11, 2018, I feel intense pain in my lower abdomen. I have a constant urge to urinate, but no burning when urinating. I wake up 6 times during the night. I think I’m dealing with a urinary tract infection. The next day, I rush to the doctor. A urine test is performed. Antibiotics and sick leave are prescribed.
From Friday to Sunday, the pain is more and more intense. Antibiotics and cranberry juice have no effect. I feel an intense pinching sensation at the level of the fibroid and twinges. All the hypotheses run through my brain. Aïssatou tells me about necrosis of the fibroid (the withering away of a fibroid caused by a drop in the blood supply) or the torsion of a pedunculated subserous fibroid.
On Monday, I am back at the medical clinic. Another doctor consults me. The results of the urine tests are negative. I inform him of the hypothesis of necrosis of one of the fibroids. Confronted, he asks me if I am in the medical field. Not at all! I’m just trying to figure out what’s going on in my body. After an abdominal palpation which provokes a high-pitched scream, the doctor assumes that it is an inflammation of the peritoneum or indeed necrosis. An X-ray or MRI is needed to make a diagnosis. He sends me to the emergency room of the hospital where I am on the waiting list for the operation.
Approached by a student doctor, I again explain my pain, the history of fibroids, the waiting list… I tell him that I am under the care of a gynecologist at this same hospital.
She tries to palpate the cervix, without success. Another student doctor joins her. I tell him the same story again. He wants to examine the cervix again. “Your colleague just did it. She wasn’t able to do it.” I tell him with exasperation. He insists. He does it. Identical result.
I ask them to contact the gynecologist who follows me in this hospital. Surprisingly, I never see him.
I ask that he check that it is not an inflammation of the peritoneum. Impossible according to them; I have no fever or vomiting. I demand an ultrasound. After 30 minutes of waiting, the 2 student doctors, accompanied by the head gynecologist and a machine to perform an X-ray, join me. After 5 minutes, the head doctor says to me: “You have large fibroids! The results of the urine test and the blood test are normal except for a slight anemia. You can go home. There seems to be nothing abnormal “.
For those who know Nicky Larson, my desire at that time is perfectly illustrated by this image. It’s a good thing I didn’t have a sledgehammer…

I insist on another ultrasound. It is out of the question that I go home without knowing the cause of my suffering. I get an appointment for the next day at the radiology department. He gives me a prescription for analgesics and anti-inflammatories to take depending on the intensity of the pain, for an indefinite period.
Before leaving, the doctor warns me: “It’s not sure whether we will see something with an ultrasound”. I reply: “Okay! In that case, what do we do?” I have no answers. I am beside myself.
By insisting for answers, I sometimes feel that my case annoys the doctors in front of me. I’m sure they’re not denying my pain, but in some way, I’m underlining their failure. They offer me no solutions, no answers.
Dozens of questions race through my brain. Will these anti-inflammatories affect my intestinal flora? What can I take to protect it? How long should I take them? How do I justify my repeated absences to my employer? Will I ever find a doctor who will listen to me and agree to operate on me? How long will it take?
To my great despair, in order to alleviate my suffering, I decide to take Fibristal for a month.
Phase 3: the week of miracles called compassion, empathy, and liberation.
I go to a private radiology clinic to perform the MRI that was prescribed to me a few months earlier. The attention and sympathy of the medical assistant touch me deeply. Even though I am surrounded by wonderful family and friends, I finally have the feeling of being helped by someone close to the medical profession. The MRI completed, I leave with the CD. I have to wait 10 days for the doctor to receive the results.
Ten days later, still on anti-inflammatories, I’m back in the gynecologist’s office. The long-awaited and well-known result falls: the largest fibroid is necrotic. At first glance, this is good news since it means that the fibroid is dying. But how long will the pain last? What can I do to reduce the intensity?
“What do we do?” I ask the doctor. I receive the answer like a stab to the body: “There is nothing we can do except take the anti-inflammatories.” he says.
The excess of tears held back for days now flow down my face. I look at the doctor and say to him: “I am not talking to the doctor, but to another human being. In front of you, you have a human being who has been suffering for 3 weeks now, who is on anti-inflammatories for an indefinite period. You are in the medical field. You know doctors who can operate on me. I can wait until April if necessary, but help me find a doctor who will operate on me. “
Three hours later, I am in front of the doctor who will operate on me in the following days. My pain has finally been heard.
On February 7 at 6:30 am, I am in the hospital to undergo the long-awaited myomectomy.
At 6:45 a.m., I’m in the taxi on my way home. The nurse informed me 5 minutes after my arrival that the obstetrician-gynecologist canceled all her interventions.
I go from relief to despair. I can’t think anymore, I’m so tired. I don’t want to fight anymore. At that time, my friend Fauve who accompanies me shows me an email she received that morning. A real balm to the heart! At 8 a.m., I call the doctor’s office to ask for another date for the operation. I learn that the doctor is waiting for his patients in the operating room. He hadn’t canceled his operations. Big administrative error! Impossible to operate on me since I had just had my breakfast. The Quebec health system is suffering, my dear friends! My suffering will have an end. But when will our health system be cured? In short, that’s a whole different story!
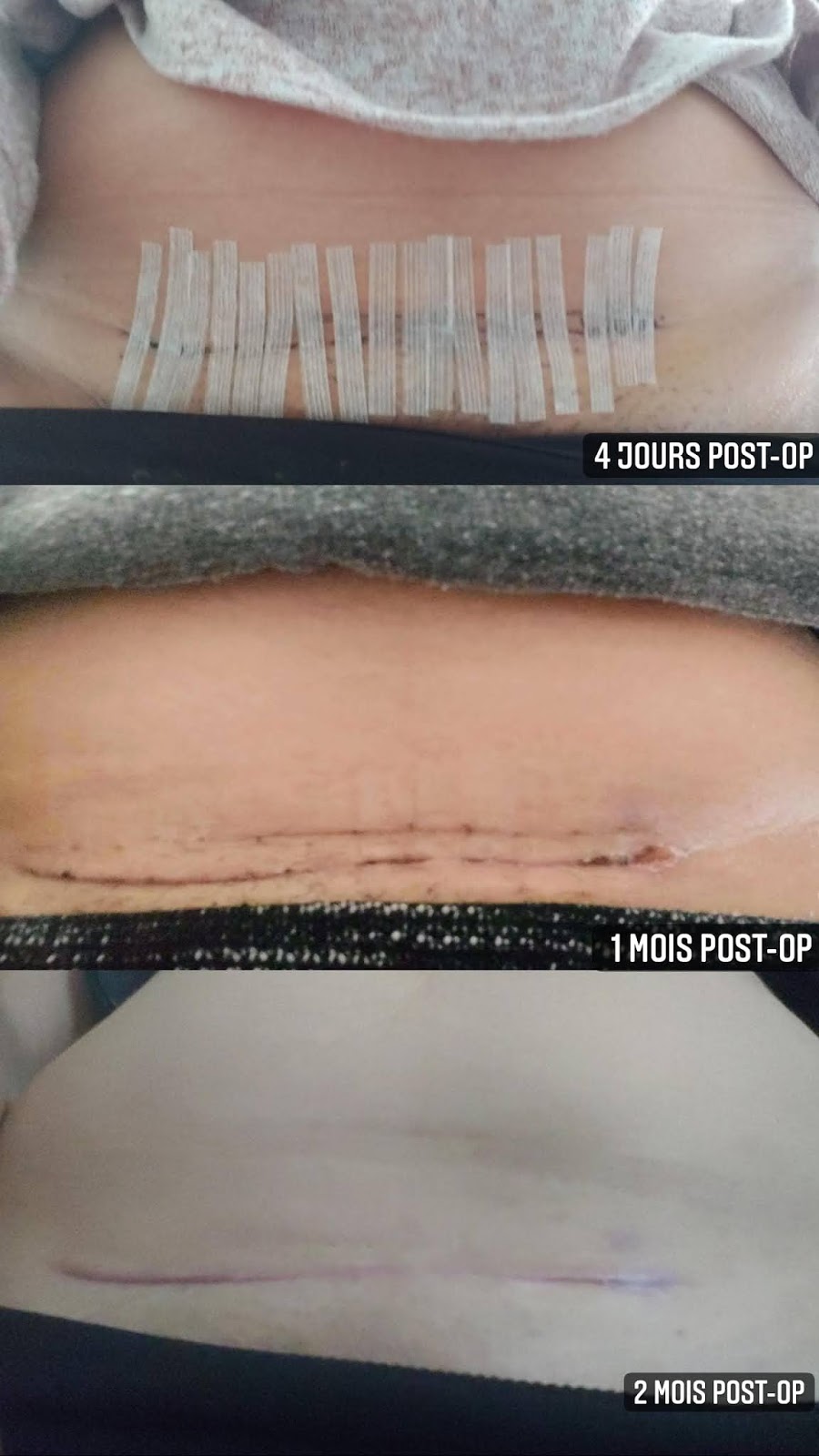
The myomectomy by laparotomy under general anesthesia took place on February 21. More than 3 hours in the operating room. A superb medical team took care of me. More than ten subserous fibroids removed. Four nights in the hospital. A beautiful scar described as a work of art by the nurses. I assure you; my scar no longer looks like that!
During my two months of convalescence I concentrated on rest, yoga, massage of the scar with essential oils, vegetable soups and aloe Vera juice.
I know fibroids can come back. But today, I am up and fighting. I would like to thank all the people who surrounded me with their love as well as the Vivre 100 Fibromes association.

Source: my niece
Make this phrase a rule of life: “If you are in severe pain or discomfort, don’t let the medical staff force you to be quiet. Stay firm because you might just save your own life.“
Never give up when it comes to your health. Listen to your body. Seek to know, to understand your illness. Inform yourself. Assemble your medical file. Knock on multiple doors. Ask for different opinions. Surround yourself with people who support you. And above all, keep hoping that a door will open.